Preimplantation genetic diagnosis
Preimplantation genetic diagnosis is used to examine the chromosomes of the embryo before it is transferred to the uterus. It can help people suffering from miscarriages, repeated failed fertility treatments or infertility caused by age, for example. Preimplantation genetic diagnosis can also be used to study the risk of serious genetic diseases.
Felicitas Mehiläinen has been using the preimplantation genetic diagnosis method since the early 2000s. With our experience and advanced methods, the outcomes of our treatment are excellent. No referral is required and treatment can be accessed quickly.
How is preimplantation genetic diagnosis performed?
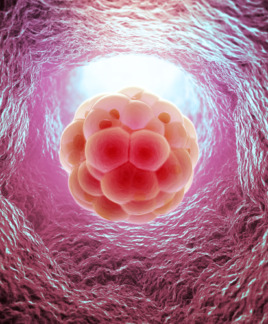
The preimplantation genetic diagnosis study is carried out in connection with in vitro fertilisation treatment, in which the embryos are cultured for 5–7 days after egg retrieval up to the so-called blastocyst stage. In the blastocyst stage, approximately 5–10 cells are taken from the embryo’s outer cell mass for diagnosis. The cells are sent to the laboratory for examination and the embryos are frozen. Embryos that are deemed to be chromosomally or genetically normal/healthy are transferred to the uterus in later sessions.
Various methods of preimplantation genetic diagnosis
Examination of abnormal number of chromosomes (aneuploidy), i.e. PGT-A analysis
A PGT-A screening study carried out in connection with IVF treatment can be used to detect chromosomal abnormalities in embryos. These abnormalities are strongly associated with miscarriages, advanced maternal age and embryo implantation failure.
Aneuploid embryos are possible in each treatment cycle, but the likelihood increases with the age of the woman. 50% of embryos can be aneuploid in women under the age of 35, while in women over 42, the degree of embryo aneuploidy can be even higher than 80%. Pregnancy can be achieved more quickly by selecting embryos with normal chromosomes for embryo transfer and cryopreservation. This treatment method is becoming increasingly popular.
Investigation of known genetic defects, i.e. PGT-M analysis
The PGT-M method allows for detecting individual genetic defects that cause serious hereditary diseases and selecting a healthy embryo to be transferred to the uterus. The method is used if the risk of diseases caused by a single gene has been identified from family history, a positive carrier result or a previously diagnosed child.
The PGT-M analysis is performed in connection with the PGT-A analysis in order to obtain both an embryo with the correct number of chromosomes (euploid) and without genetic defects related to the disease in question.
Investigation of hereditary chromosomal abnormalities, i.e. PGT-SR analysis
The PGT-SR method examines abnormalities in the number (quantitative) or structure of chromosomes and it can detect, for example, a situation where the number of chromosomes is normal, but parts of two different chromosomes have switched places (translocations).
The PGT-SR analysis is used if a healthy parent has a balanced
translocation or inversion (a part of the chromosome is reversed). In this case, however, a structural abnormality in the gametes may be unbalanced, which can lead to reduced fertility and miscarriages.
The PGT-SR analysis is performed in connection with the PGT-A analysis in order to obtain both an embryo with the correct number of chromosomes (euploid) and without structural abnormalities.
Examination of embryo chromosomes from culture medium, i.e. niPGT-A analysis
In some cases, it is possible study the chromosomes of the embryos with the culture solution. In the niPGT-A method, embryos are scored and an order of embryo transfers is established. The normal PGT-A and niPGT-A methods are approximately 80% equivalent, which means that aneuploid embryos cannot be fully avoided with this method. However, the method makes it possible to achieve pregnancy more quickly.
Embryos are cultured for six days for the niPGT-A analysis, after which the culture medium is collected and sent to the laboratory for examination and the embryo is cryopreserved. The biggest advantage of the method is the lack of need for an invasive embryo biopsy, which means that there is no need to take a sample from the embryo.